Effective disease management depends on early and accurate diagnosis of XLMTM
XLMTM diagnosis versus other neuromuscular disorders
Clinical suspicion of X-linked myotubular myopathy (XLMTM) can be challenging due to similarities with other neuromuscular disorders.1 Recognizing key clinical features of XLMTM and early genetic testing can accelerate diagnosis.
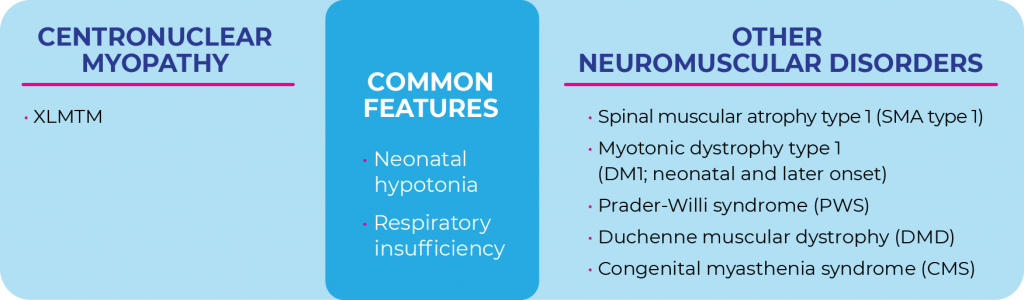

Unlike other neuromuscular disorders such as spinal muscular atrophy (SMA type 1) in which symptoms can manifest any time from birth to 6 months, most patients with XLMTM present at birth with profound hypotonia and respiratory insufficiency.1-4
If you suspect XLMTM and need help in establishing a diagnosis, download this differential diagnosis educational resource for neuromuscular disorders.
Suspicion of XLMTM may be based on family history and clinical findings
In addition to profound hypotonia and respiratory insufficiency at birth, these combined common features can assist in the differential diagnosis process1:
- Facial weakness
- Dolichocephaly (length and head circumference greater than 90th percentile)
- Ophthalmoparesis, often associated with ptosis
- Long fingers and toes
- Bulbar weakness leading to insufficient sucking and swallowing
- Frog leg position with abducted hips and flexed knees
- Areflexia (abnormal or absent reflexes)